In October 2021, ArteraTM released a report, “Clinical Support Staff Burnout Linked to Patient Communication Challenges,” an in-depth study measuring staff burnout in healthcare for clinical support staff.
The purpose of the study was to examine what negative effects burnout was causing on those workers who many consider to be the backbone of the U.S. healthcare system. Additionally, the study also explored the role patient communications plays in relation to clinical support staff burnout.
Released in October 2021, the study uncovered that clinical support staff were overwhelmed and frustrated by spending hours each day, manually communicating with patients via phone. In fact, 88% of those surveyed reported moderate to extreme burnout so severe it caused many workers to want to quit. The study also explored new areas including how digital patient communications is seen as an important tool to reach underserved populations and increase access to care overall.
Conducted during the peak of the COVID-19 pandemic, the 2021 results were not surprising since the first two years of the pandemic pushed all medical staff to their limits. In addition to major disruptions to in-person care, there were mandatory new regulatory requirements brought on by the pandemic and the stress created by ineffective patient communication during these challenging times. All these factors led to epic levels of medical staff burnout, and clinical support staff was no different.
Clinical support staff, many of whom are tireless office workers, are responsible for communicating and coordinating with patients. Other support tasks are scheduling appointments, facilitating test results, handling billing questions, and anything and everything that insures providers can focus on delivering high-quality patient care. It’s indisputable the COVID pandemic changed so much in the healthcare system, yet three years post the onset, the industry has been able to adjust to a new normal. A factor in the ability of healthcare to adapt to this new normal is due to a surge in digital innovation. From telehealth to patient communications to clinical communication software, digital tools have enabled healthcare to continue conducting business as usual, and in some cases, innovating many of its outdated processes.
Clinical support staff burnout-one year later
Even though patient care in the U.S. is the most advanced in the world, patient-provider communications continue to be a challenge. The U.S. healthcare industry is notorious to have one of the worst-rated communication experiences of any industry. Despite efforts by many providers to move to patient-centered care models, healthcare communication processes still often fail to meet patients on their terms.
Curious to see what a difference a year makes and how digital trends continue to affect clinical support staff, Artera conducted a new study of over 300 clinical support staffers across various health systems who are responsible for communicating with patients. The study was conducted by PureSpectrum, an independent market research platform that gathers insights online. PureSpectrum surveyed more than 300 clinical support staff who are responsible for communicating with patients, which can include nurses, physician assistants, front desk/reception, and other medical professionals communicating directly with patients.
Released in December 2022, this latest study, The State of Clinical Support Staff, looks at clinical support staff burnout, its impact on patient care, and trends in patient communications. The updated report discovered clinical support staff burnout is still high but on the decline and while levels are nowhere near acceptable, the Artera report found that fewer clinical support staff are at their breaking point as digital patient communication technology is being adopted more and more.
“The report reinforces what we consistently see with our customers: digital patient communication can save staff time, improve their wellbeing and enhance patient care,” said Guillaume de Zwirek, CEO and Founder, Artera.
The impact of burnout on clinical support staff today
Artera’s 2022 study found that although clinical support staff burnout remains high, it is lower than it was during the peak of the pandemic. Seventy percent of those surveyed report moderate to severe burnout, with 32 percent rating it as high or severe. This is down from the 2021 report where 88 percent reported moderate to severe burnout and 56 percent reported high or severe burnout. Thirty-three percent of clinical support staff reported their burnout negatively impacted their quality of patient care while 41% say their burnout has even been noticed by a patient. In a sobering statistic, 43% report at least one instance where poor or ineffective patient communication negatively impacted a patient’s health.
Despite the continuing high levels of staff burnout, 30% fewer people (33% of study respondents) reported wanting to quit because of burnout compared to last year’s study where 63% reported a desire to leave their jobs. Interestingly, the recent study found that only 47% reported their burnout to their supervisors, which is 23% less than the 2021 study where 70% said they shared their concerns with their managers. Management response was 20% lower in 2022 with only 60% of managers responding to workers’ concerns versus 2021, where 80% responded.
Poor patient communication is the key reason for staff burnout
When asked about reasons for their burnout, a majority (56%) of clinical support staff cited poor patient communication as a direct cause of their burnout. Seventy-one percent of those surveyed reported phone-based patient communication to be a source of frustration for many clinic support staffers, with many spending hours each day coordinating and communicating with patients. Sixty-eight percent reported they are spending two hours or more every day on patient communication while one-in-five (20%) said they spent an extraordinary four or more hours. The study also found that 63% believe that communicating with patients only via phone creates unnecessary barriers for patients from lower income levels, those from underserved populations, and patients who speak English as a second language.
Although in the recent study, 56% of clinical support staff attributed patient communication as the reason for their burnout, on a positive note, this is down from 82% in 2021. The new lowered number is likely due to the growing adoption of digital patient communications tools. Forty-eight percent in the 2022 survey reported texting, emailing, and digitally messaging with patients more frequently than they did in the early days of the pandemic. Only 17% said they used fewer digital tools than in 2021. Similarly, while the 2021 study found that nearly all clinical support staff (97%) were using the phone as their primary method of patient communication, that number dropped to 85% this year.
Digital patient communications tools mitigate staff burnout in healthcare
Clinical support staff believe innovative patient communication technology not only makes their lives easier but they also make their patients’ lives better. The survey discovered that 64% of clinical support staff believe that digital patient communication tools would allow patients to engage more in their own health while 78% believe these tools would increase access to healthcare. Sixty-seven percent agreed digital patient communication would help address disparities for underserved patients. Seventy-one percent of the survey respondents believe digital patient communications would help address social determinants of health for their patient populations.
For certain patient populations, there are language barriers or due to jobs and other commitments, these patients aren’t available to speak on the phone with providers during regular office hours. In the 2022 ArteraTM study, 74% of clinical support staff said they experienced that portions of their patient populations were unable to communicate during their office hours. In fact, of that group, approximately one-third (31%) estimate that half or more of their patients face difficulties communicating during regular office hours. Additionally, 76% reported their healthcare system struggles to communicate with some patients in their preferred language. When asked if communicating with patients in their preferred language will improve healthcare access overall, 85% responded yes.
Addressing the economic security threat of staff burnout in healthcare
Staff burnout is being recognized as a key crisis in the healthcare industry to the point that the 21st Surgeon General of the United States, Vivek Murthy, wrote an article on health worker burnout for the New England Journal of Medicine stating, “Health worker burnout is a serious threat to the nation’s health and economic security.”
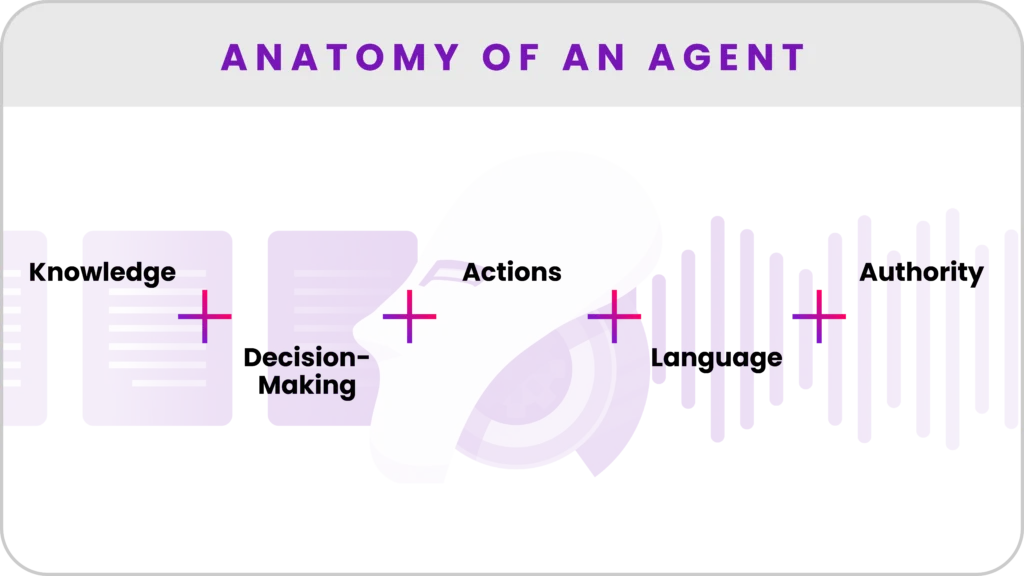
As demonstrated by the findings of the 2022 State of Clinical Support Staff study, progress has been made in addressing staff burnout in healthcare but there remains room for significant improvement. The key findings in this report suggest one of the biggest factors in alleviating clinical support staff burnout is the use of digital patient communication tools which help to ease staff workloads by automating time-consuming patient communication, eliminating the need for phone calls and other repetitive tasks.
The results of the 2022 study are in accordance with the Surgeon General’s recommendations for key interventions to tackle staff burnout which include promoting safe workplaces, addressing staff mental health, better wages, and reducing administrative burden.
The time for bold change in the healthcare industry is now. To alleviate the staff burnout in the healthcare crisis, we must take care of our workforce and leverage innovative technologies so that medical and clinical support staff can focus on patient care and other high-value tasks which originally inspired them to pursue a career in healthcare.♥