SHARE:
[DISPLAY_ULTIMATE_PLUS]
The gap between what we say we’ll do — hike the trail — and what we actually do — hit the couch — matters. A lot.
According to the CDC, up to 40 percent of annual deaths from each of five leading U.S. causes are preventable.
But we can’t improve health outcomes for patients with many of the most chronic conditions and prevent new ones from arising if we can’t change patient behavior. That requires influencing the choices patients make about entrenched behaviors.
“In the past, physicians’ way of treating the behavioral part has been to say something like, ‘You really should stop drinking,’” said Colleen Christmas, Director of the Internal Residency Program at Johns Hopkins Bayview Medical Center. Not surprisingly, the success rate for that intervention wasn’t very high, she said.
Today we know that fear-based warnings have little power to change patient behavior. Instead, positively-grounded approaches that tap into our human tendency to feel in control, confident and connected to others trigger action.
Mobile technology can empower patients to make healthier choices at scale, but only if the tools are based on social science research and health behavioral models. Otherwise, patients are likely to ditch tech-driven change programs as quickly as the latest fad diet. Here are key science-backed strategies that work best to shift patient behavior.
1. Help patients set meaningful goals and plans with assessments
“What matters to you?” in the context of health is one of the most powerful questions a healthcare professional can ask a patient because it places them in the driver’s seat.
Unearthing what the patient values and what realistic goals will inspire them, however, can sometimes take longer than a 15-minute visit.
With mobile technology, you can ask the patient more questions through text or messaging to help determine goals and plans they’ll fight for because they are personalized to the patient’s unique preferences, values, and needs.
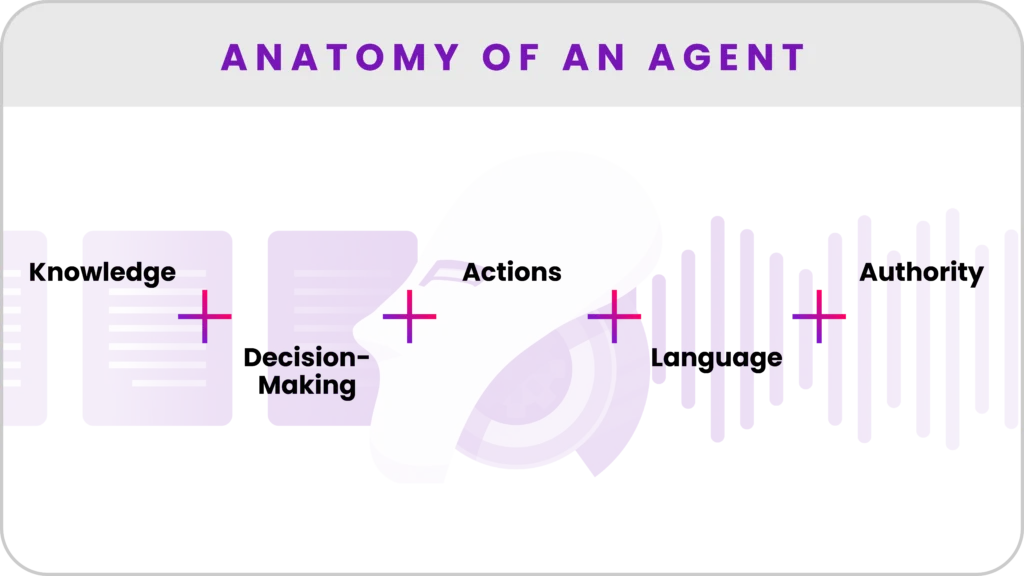
2. Increase patients’ knowledge
“Patient behavior is driven by fear of the unknown,” says Dr. Kevin Pho. And this fear causes patients to freeze, not act.
But you can educate patients about a new mindset and behavior by texting them links to how-to videos or reinforcement quizzes. This information increases their sense of autonomy, competency and the likelihood they will take action. Knowledge is a powerful predictor of behavioral change.
3. Provide coaches and care team support
Patients struggle to stick with a new behavior when the emotional side of the brain becomes exhausted trying to wrestle with a nearly automatic action (e.g., a morning cigarette with coffee) and self-control plummets, according to Chip Heath and Dan Heath, academics and authors of Switch: How to Change Things When Change Is Hard.
As a result, patients need more than a care team member following up with them every few weeks or months; they need ongoing check-ins, reminders and encouragement to stay on track. Numerous studies demonstrate that health professionals and coaches who cheer and counsel help.
With automated texts or one-to-one messaging, you can provide patients with this critical day-to-day support. You can also pro-actively intervene when patients slip from their regime.
4. Connect patients to peers
In addition to emotional support from family and friends, peer-to-peer groups (both in-person and virtual) are powerful at aiding behavioral change. Research shows that patients with the same health condition who interact with each other have better outcomes. The element of social pressure — wanting to conform to what others do and do it better — drives action.
The problem is time-strapped patients can’t always attend in-person groups, assuming they exist. Virtual groups and social communities, however, allow patients to engage and connect in ways that work best for them.
5. Provide immediate praise
Patients should be recognized or rewarded for making progress in achieving their health goals instantly.
Why? According to neuroscientist Tali Sharot, when a behavioral change, such as taking medication at a specific time, becomes associated with an instant reward, adherence is more likely to become a habit.
Without certain technologies, however, it’s nearly impossible to always know when a patient has succeeded at a task, such as taking a daily walk. As a result, you can’t congratulate them at that moment, which might be 5:30 a.m. on a Saturday.
However, a texting program can ask a patient if they have completed a loop around the neighborhood. If they confirm, the system can text back a “you’re-crushing-it” emoji or a reward. Positive, real-time feedback motivates.
Here are three examples of how mobile programs grounded in behavioral theory are making it easier for patients to take better care of themselves.
Teens quit smoking at double the average rate with SmokefreeTXT
Although the majority of teens want to kick their smoking habit, only 2 to 3 percent are smoke-free six months after quitting on their own.
The SmokefreeTXT program, led by the National Cancer Institute, has managed to double this dismal cessation rate by sending 13- to 19-year-olds text messages that contain behavioral treatment elements.
The user begins by selecting and texting a quit date, which elicits a feeling of being in charge. The program then asks the user questions around mood, craving and smoking status. After assessing the responses, the program texts back tailored content that instantly praises progress or empathizes with the user’s difficulties, eschewing a shame-based approach.
For example, if a user texts that they crave a cigarette, the program sends actionable tips, such as “do jumping jacks” and a “stay strong!” message. And to stave off future cravings, they receive follow-up texts, such as how to identify their top three triggers.
Behavioral scientists designed the program. It has succeeded where others have failed by meeting teens where they are. It incorporates personalized goals such as quit date, along with knowledge and praise.
A “change your brain, change your body” app helps patients lose weight
For the 86 million Americans with prediabetes, hitting weight loss goals has taken on a new level of urgency.
One thing seems to be helping them make healthier choices: the Noom diabetes prevention app.
A study published in 2016 in the British Medical Journal Open Diabetes Research & Care found 64 percent of participants who completed Noom’s 24-week program lost over 5 percent of their body weight. They were also highly engaged with 84 percent completing the program.
On the heels of this study, Noom became the first virtual provider to receive full recognition from the CDC.
Why has the program worked?
“Ultimately, we wanted to tackle what everybody was failing to address: the psychology of health behaviors,” said Saeju Jeong, CEO of Noom.
Indeed, Noom focuses on the mental and social side of weight loss and injects an element of fun. Users of the app message with human coaches and swap information and stories with other “Noomers” in virtual support groups. They also complete daily to-do lists based on their personality and preferences and read short health and psychology lessons.
By including the key elements known to spark behavioral change, Noom appears to be making headway in reducing the chances of users progressing to type 2 diabetes.
Breast cancer patients’ stress decreased with text support
Just over half (51 percent) of patients don’t remember advice their physicians give them unless prompted, while others may hesitate to ask certain questions.
For those patients undergoing chemotherapy who are trying to navigate a multitude of side effects on their own, these information gaps can cause anxiety.
Fox Chase Cancer Center conducted a randomized study with women diagnosed with breast caner. One group of women received a booklet on chemotherapy. The other group received daily text messages.
The texts asked them if they wanted information on how to manage symptoms, such as fatigue and neuropathy. Patients were also able to text the program with questions about their treatment.
The 48 women in the texting group sent more than 8,000 texts seeking information. More importantly, they reported decreased symptom distress and increased quality of life compared to those who were only given the booklet.
“Women felt like they were getting bursts of information over time rather than all at once and it was always on their phone to go back and look at,” said Kuang-Yi Wen, Assistant Professor in the Cancer Prevention and Control program at Fox Chase Cancer Center and lead author of the study. “They want to feel supported, empowered, and in control.”
Researched-backed strategies work
When based on behavioral theory, mobile technology’s ability to personalize content, provide support and connect patients at scale can nudge them to healthier choices and better days ahead. ♥