When it comes to digital patient engagement, healthcare providers are walking a tightrope. On one side, standardization offers consistency, reduced costs and seamless scalability across systems. On the other, innovation drives differentiated patient experiences, improved access and increased engagement. But how can healthcare providers strike the perfect balance between these seemingly opposing principles?
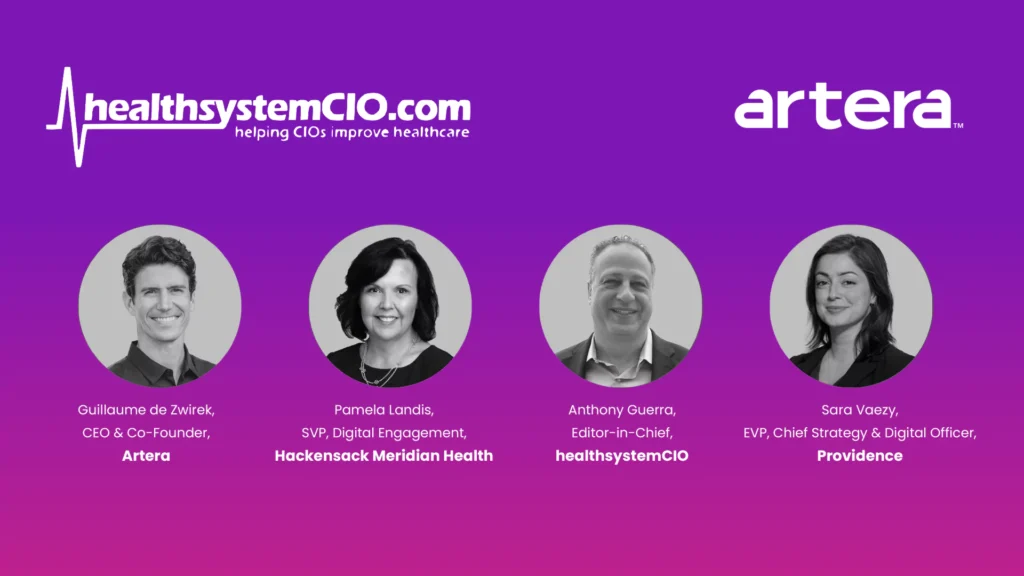
This question was at the heart of a recent Artera-sponsored webinar hosted by Anthony Guerra, Founder and Editor-in-Chief at healthsystemCIO. The panel included industry leaders Sara Vaezy, Chief Strategy and Digital Officer at Providence, Pamela Landis, Senior Vice President of Digital Engagement at Hackensack Meridian Health, and Guillaume de Zwirek, CEO of Artera.
Their insights not only provided meaningful answers to this challenge but also offered actionable steps providers and health tech innovators can take to create a cohesive digital patient engagement strategy.
Below, we break down the key takeaways from the discussion, focusing on innovative differentiators, care gap closure and steps to get leadership buy-in on next-generation technologies that will drive results – both in terms of outcomes and finances.
Differentiation Matters
The digital health landscape continues to evolve rapidly. Patients now expect their healthcare experiences to match the seamless, on-demand quality of consumer brands like Netflix or Amazon. Platforms designed for digital patient engagement must balance meeting these expectations with the pressing need for standardization to ensure operational consistency and cybersecurity across enterprise health systems.
Yet, as Sara Vaezy noted during the panel, standardization and innovation aren’t necessarily opposing forces. When aligned with clear goals such as improving access and reducing friction in the patient-provider relationship, they become complementary tools. “You can standardize where differentiation doesn’t matter, but must invest in innovation where personalization and experience can make a real impact,” Vaezy explained. “From our perspective, you really need to invest in differentiation – you don’t want to have the same stuff everybody else has.”
The panelists agreed that differentiation matters when it comes to acquiring and retaining patients. “I don’t want to look like everybody else in our market,” Landis said. “You don’t compete by looking like everybody else.” She believes patient loyalty isn’t just about the quality of care—it’s about access, ease and personalization. “Patients are loyal to their doctors, not necessarily their health systems,” Pamela stressed. “Our job is to use technology to strengthen those relationships. I always think: ‘What’s going to make it easier for patients and our clinicians to have a better relationship with each other?'”
Patient-Centric Innovation Drives Long-Term Engagement
Guillaume de Zwirek expanded on this, explaining how technologies that streamline patient access, appointment scheduling and engagement create differentiation in competitive markets. By deploying solutions that focus on simplicity and immediacy, health systems don’t just meet expectations—they exceed them. He also believes healthcare is stepping into a more bundled approach, similar to how digital streaming channels have started to partner – Hulu and Disney Plus, for example.
Ultimately, providers are looking to leverage fewer vendors while getting them to do more – that’s the easiest way to cut costs – for the time being. That being said, the long-term ramifications of these type of decisions could be detrimental in the long-run, de Zwirek believes.
Vaezy agrees that health systems will likely see the consequences of a consolidated tech stack in 6-12 months, noting that providers may be “getting a platform to do a little bit of everything, but nothing super well.” If health systems choose to go another route, investing in differentiated patient engagement tools, the challenge remains to showcase clear ROI. Landis agrees:
“Patient experience should not be sacrificed to check a box for tech stack standardization. In fields like radiology or cardiovascular systems, we demand excellence, ensuring tools meet both clinical and business needs—why should patient engagement be any different? As an industry, we haven’t fully cracked the code on delivering tools that truly empower patients. While progress is being made, most tools today simply provide access to past care information—lab results, clinical notes—but fail to guide patients on what to do next. Moving forward, we need tools that help patients understand, access and manage their care proactively.”
Pamela Landis, SVP, Digital Engagement, Hackensack Meridian Health
Making the Case for Digital Patient Engagement Solutions
From the vendor perspective, de Zwirek is eager to know how technology builders can help health systems make cases internally for differentiated tools. One of the biggest barriers to innovation isn’t the technology—it’s getting buy-in from internal stakeholders, particularly CIOs and CFOs.
According to Landis, one of the ways to do so is by tracking outcomes and proving a technology’s ROI, including care gap closure. “With Artera, we’re able to prove that we’re closing care gaps, improving quality and increasing patient engagement – all while reducing no-shows and scheduling more patients for essential preventive care like annual wellness visits, mammograms and colorectal and lung cancer screenings. We’ve been able to successfully track these outcomes, clearly demonstrating the bottom-line impact and marketing lift, showing the difference between inaction and the results achieved with personalized outreach.”
Landis also shared a compelling story about a patient who scheduled a mammogram due to a text reminder, leading to early detection and treatment that saved her life. “Don’t discount the power of a story of an individual patient that you’ve helped make better – that still appeals to our CFOs and other leaders in our C-Suite. We have to show every single time the value of how a tool improved care and grew our patient base.”
In addition to sharing a patient story, Vaezy believes having a data-driven tool that can measure and quantify attribution is critical to driving further investment, as it helps to tell the top line story. She also believes having an open ecosystem and greater interoperability – encouraging greater data exchange with APIs across a tech stack – will be beneficial to all. “Everything sort of operate in silos, preventing us from consolidating the gains of the technologies we’re investing in. We can actually make the case for having some of the best of breed technologiees if they can talk to other parts of environment.”
Landis believes a good analogy for this is the banks, as they developed an open infrastructure, allowing consumers to put their cards in any ATM, allowing them to access their money from wherever. “In the end, they put the customer first. I think in our industry, we have to get to a similar point.”
Tips for Making the Case:
- Use patient anecdotes alongside data to appeal to leadership’s analytical and emotional sides.
- Quantify the downstream impact of innovations, such as increased capacity, patient satisfaction, or care gap closure.
- Consider going “at-risk” as a vendor—offering pay-for-performance models to share the financial impact of implementing new technology.
Where to Go from Here: Prioritize Growth
While the C-suite may naturally tend to go toward standardization – in light of reducing costs – Landis believes “You do not cut your way to financial stability – you have to grow your way to differentiate yourself and to take care of your patients.” While the C-suite wants to be innovative – and to do the right thing – it’s on the operators to show them how it can be done. Showcasing the difference between inaction and personalized, targeted outreach will be critical when making the case to innovate.
Balancing standardization and innovation is a nuanced process, requiring collaboration between IT leaders, clinical teams and external technology partners. However, the reward is clear—health systems that find the right equilibrium will foster better patient loyalty, engagement and outcomes in an increasingly competitive landscape.
If you’re interested in learning more about how leading healthcare organizations are navigating these changes, check out the full webinar recording to tap into specific strategies that can help your organization thrive, here, or read the healthsystemCIO recap, here.